1 The Paris Endoscopic Classification for Superficial GI Lesions
In 2002, an international group of endoscopists, surgeons, and pathologists gathered in Paris to develop the endoscopic morphological classification for “superficial” neoplastic lesions in the esophagus, stomach, and colon [1]. A neoplastic lesion is considered “superficial” when its endoscopic appearance suggests that it has not penetrated the digestive wall beyond the submucosa. In Japan, neoplastic stomach lesions that appear “superficial” during endoscopy are classified as “type 0” subtypes. The term “type 0” was chosen to distinguish the classification of “superficial” lesions from the Borrmann classification, which was proposed in 1926 for “advanced” gastric tumors and included types 1 to 4. The endoscopic morphology of superficial lesions is associated with invasive potential and can help determine treatment strategies [2].
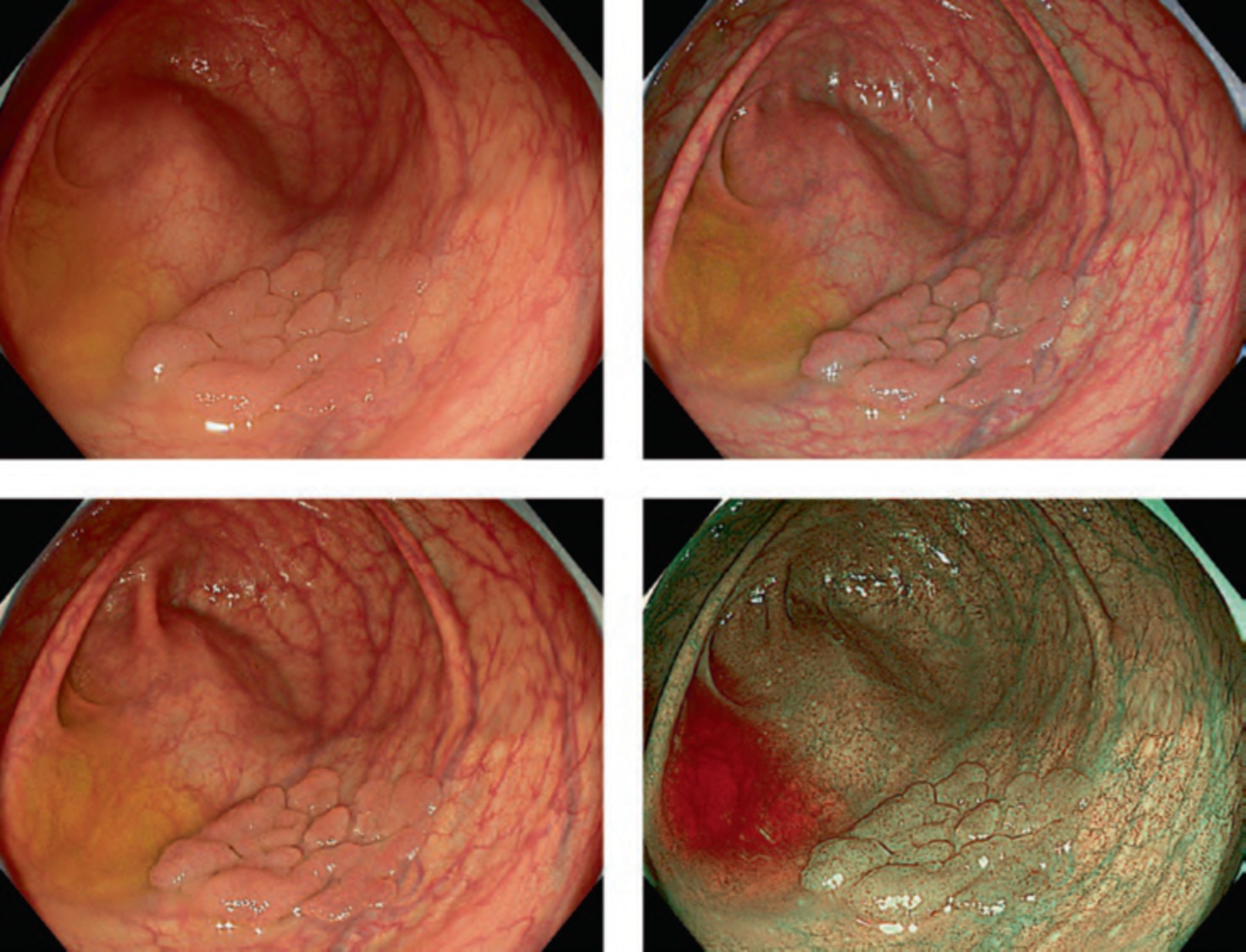
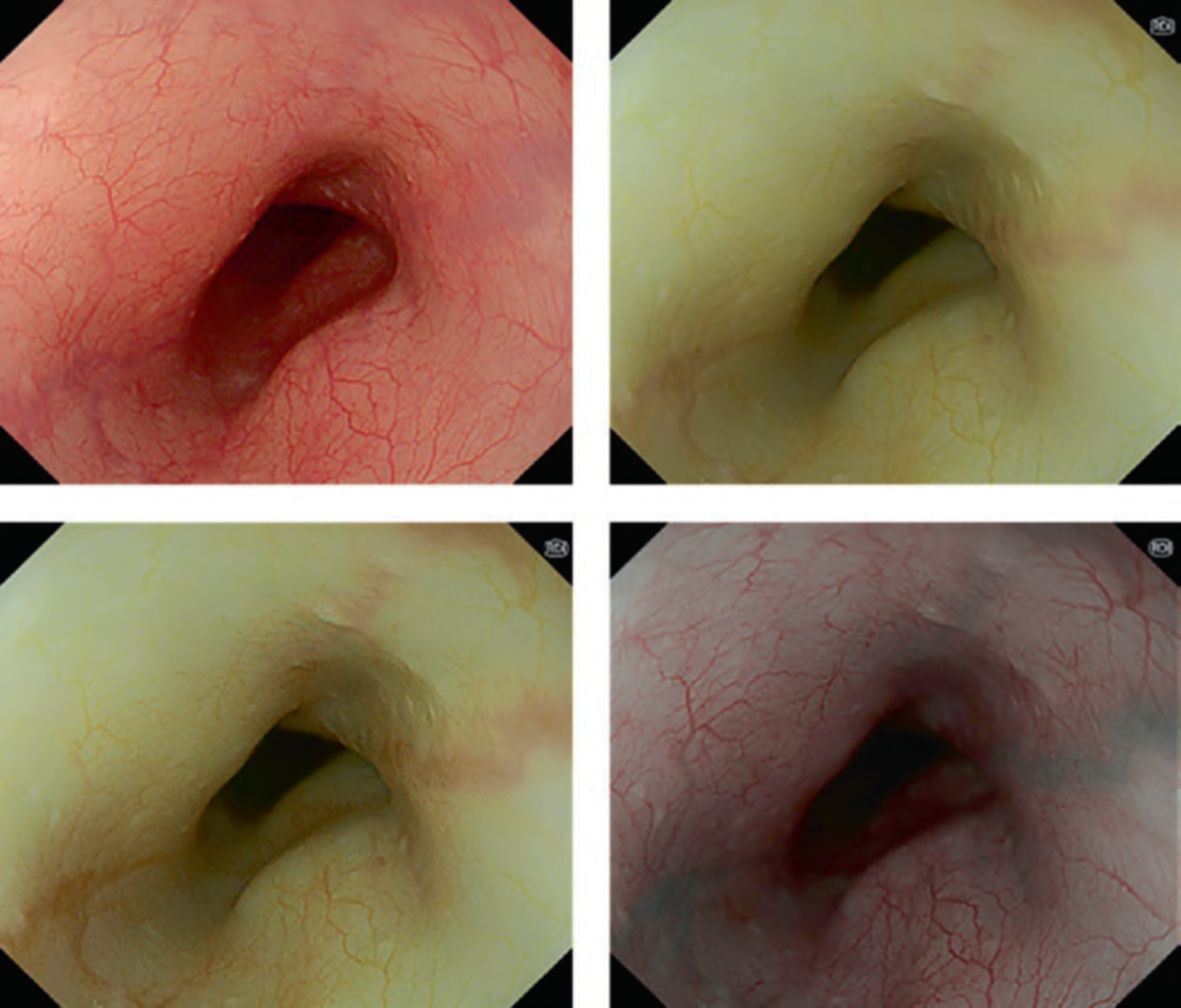
2 Definition of Endoscopic Morphology (Fig. 1)
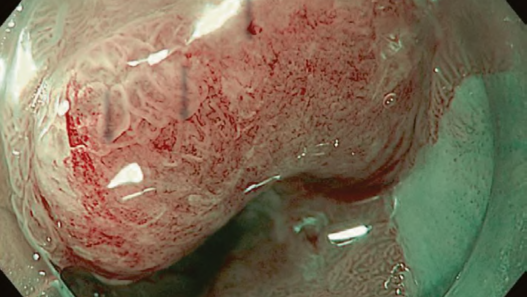
The classification of type 0 lesions is based on the distinction between polypoid (type 0-I); non-polypoid, nonexcavated (type 0-II); and non-polypoid, excavated (type 0-III) lesions. In addition, type 0-II lesions are further divided into three types, including slightly elevated (type 0-IIa), flat (type 0-IIb), and slightly depressed (type 0-IIc). Type 0-I is subdivided into pedunculated (Ip) and sessile (Is). The differentiation between type 0-I and type 0-IIa is based on the height of the closed cups of biopsy forceps (2.5 mm). Lesions protruding above the level of the closed cups of a biopsy forceps are classified as type 0-I; those below this level are classified as type 0-IIa.
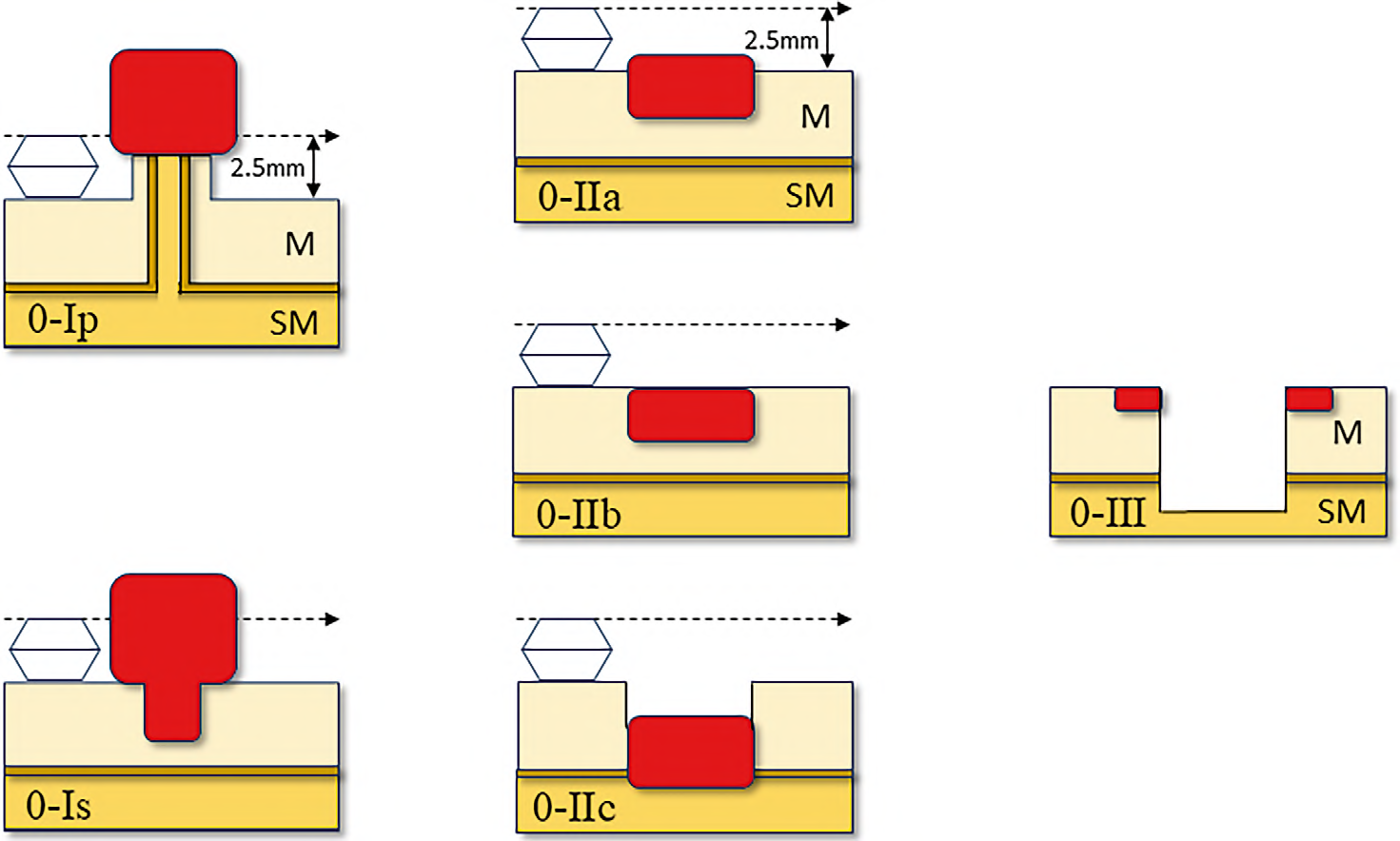
Mixed types associate two distinct types of morphology. The most common pattern of mixed types consists of an elevation (IIa) and a depression (IIc). An elevated lesion with a central depression at its top is classified as type 0-IIa + IIc. In comparison, a depressed lesion with elevated borders or a central elevation is classified as type 0-IIc + IIa. Other mixed types include type 0-IIc + Is, 0-Is+IIc, 0-IIc + III, and 0-III + IIc. However, the exact placement of this mixed-type classification requires a precise evaluation of the morphology, and there is room for interobserver disagreement because the relative surface of each type is not the only factor relevant to prognosis.
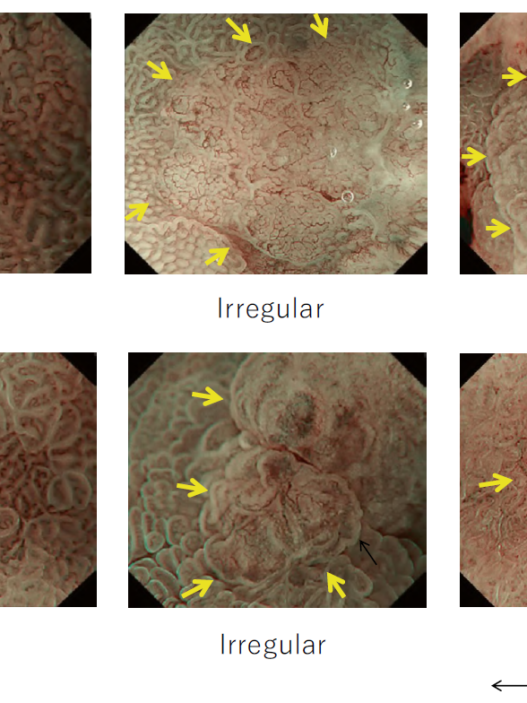
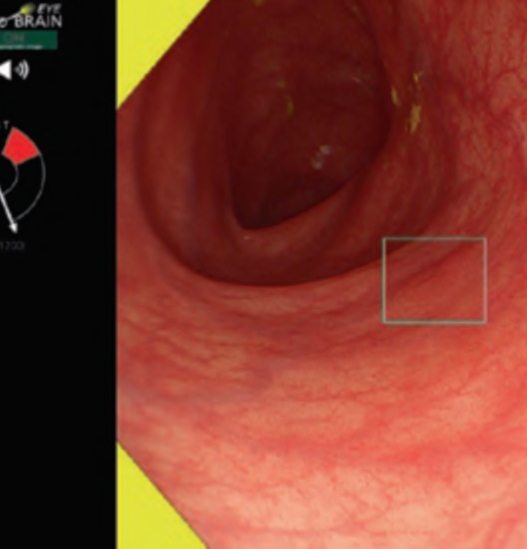
3 Endoscopic Staging
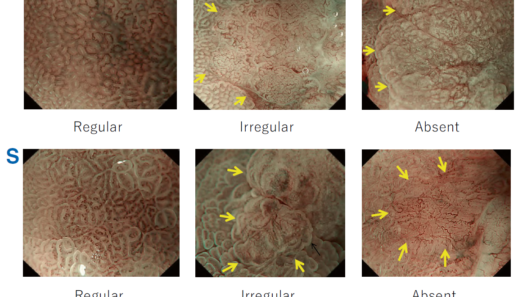
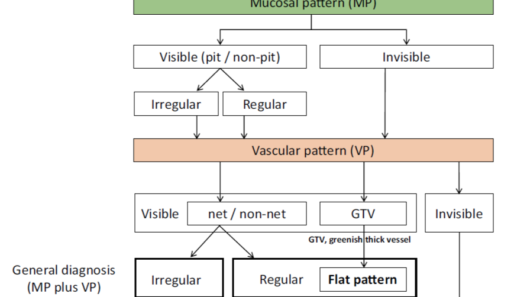
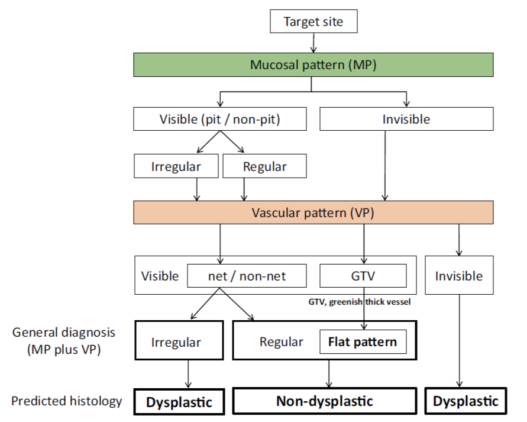
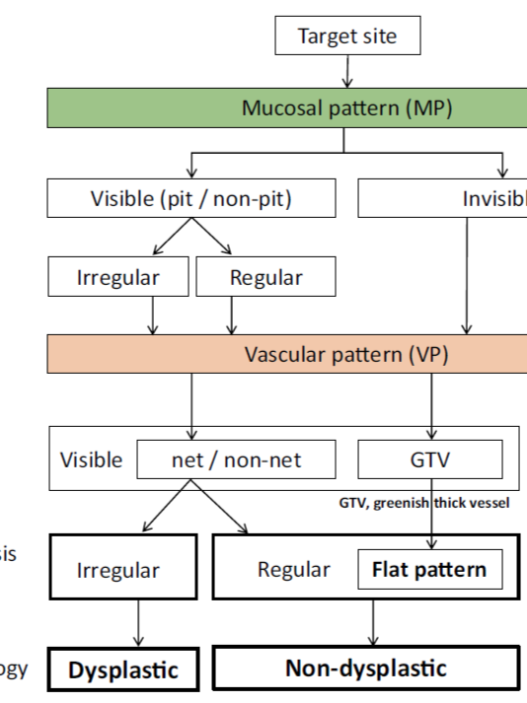
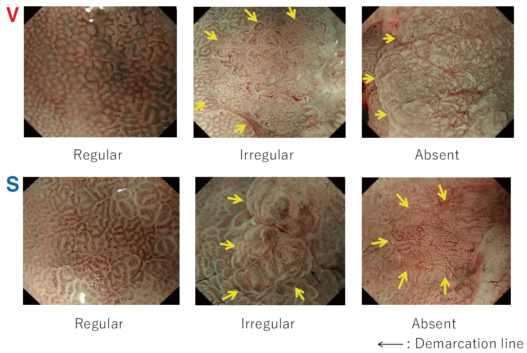
The morphology of a type 0 neoplastic lesion can predict the depth of invasion into the digestive tract wall, providing an “endoscopic staging.” Therefore, endoscopic descriptive morphology can help treatment decisions involving endoscopic resection or surgery. The primary role of endoscopic staging is to predict the risk of submucosal invasion and the associated risk of nodal metastases. For a type 0-I lesion, the size is a reliable predictive criterion. The risk of submucosal invasion increases as the size is larger. On the other hand, with type 0-II lesions, the morphologic subtypes have greater importance. Submucosal invasion is more frequent in depressed lesions (IIc) comparing the same size [3]. Mixed-type lesions are more likely to invade into submucosa at a higher proportion than non-mixed-type lesions. As a rule, type 0-IIa + IIc lesions have a poorer prognosis, with a risk of deep invasion in the submucosa. Because morphological endoscopic staging is not accurate enough, following advanced diagnoses such as chromoendoscopy, image-enhanced endoscopy, and magnifying endoscopy is required for better staging.