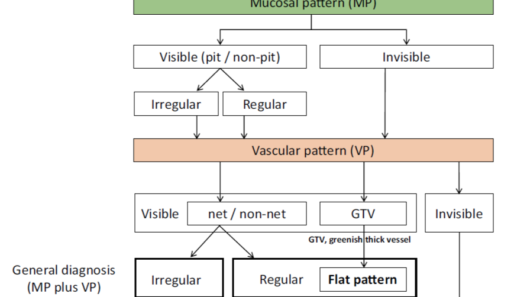
Vessel Plus Surface (VS) Classification System
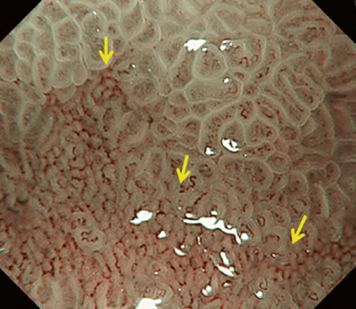
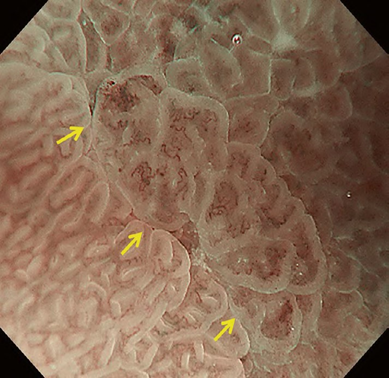
The VS classification system developed by the author (Kenshi Yao) [1] is the most widely accepted diagnostic system for magnifying narrowband imaging (M-NBI) of the stomach [2]. The VS classification system employs anatomical terms as endoscopic markers for analysis. Anatomical components visualized using M-NBI were divided into microvascular (MV) and microsurface (MS) patterns. As shown in . Fig. 1a–c, the subepithelial capillary and collecting venule were visualized for MV pattern, while the marginal crypt epithelium (MCE), crypt opening (CO), and intervening part (IP) between the crypts were identified for the MS pattern. In addition, in terms of the pathological status, the light blue crest [3] and white opaque substance [4] can be markers for microsurface patterns.
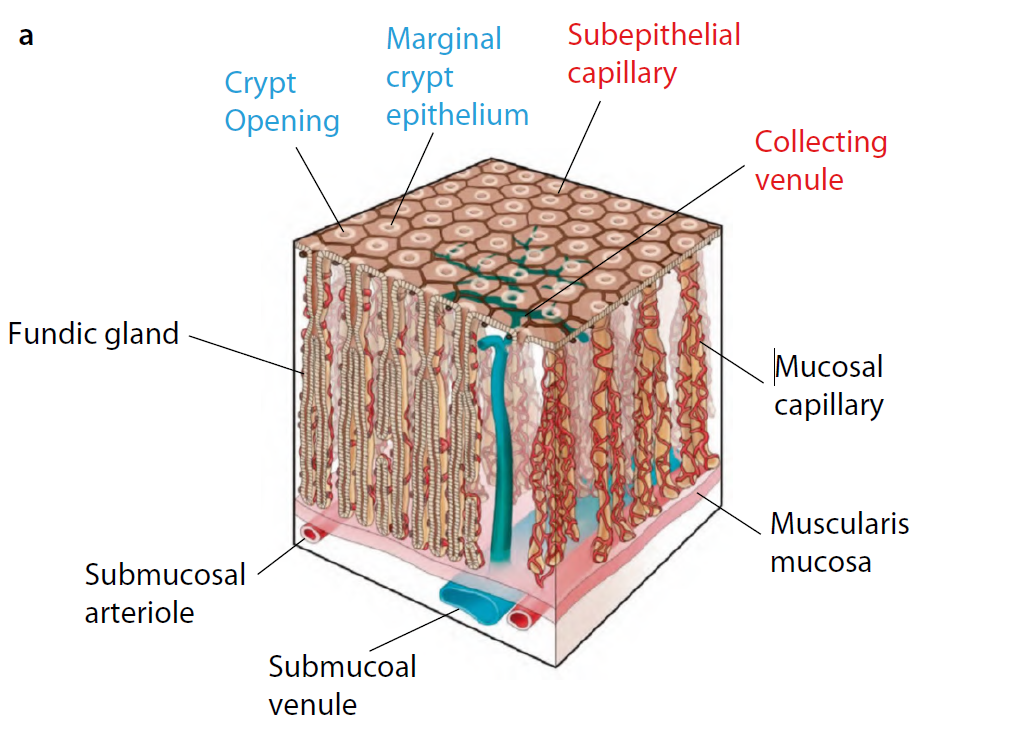
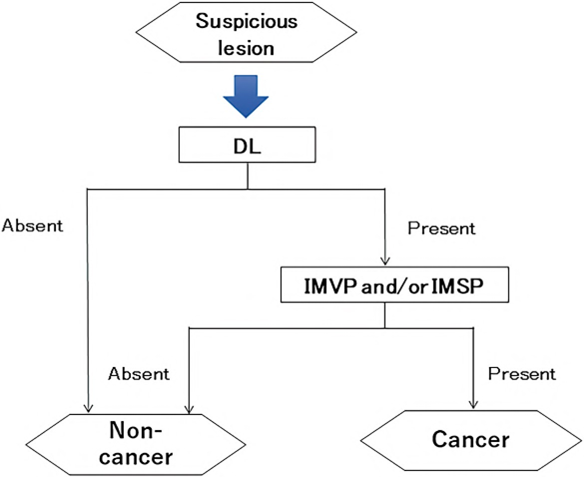
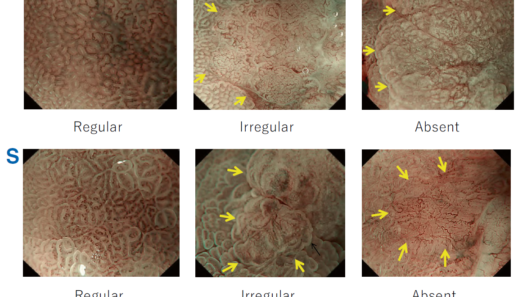
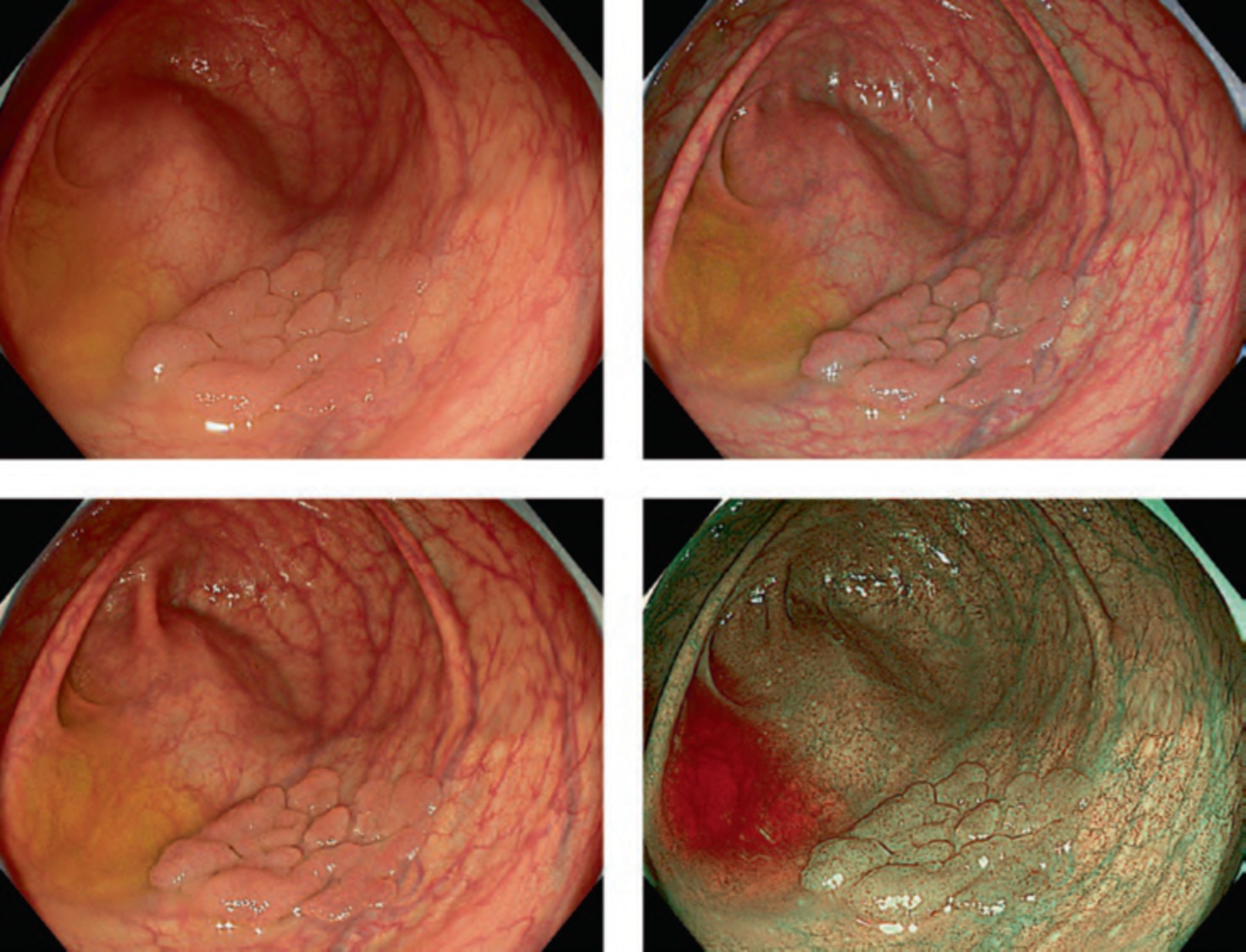
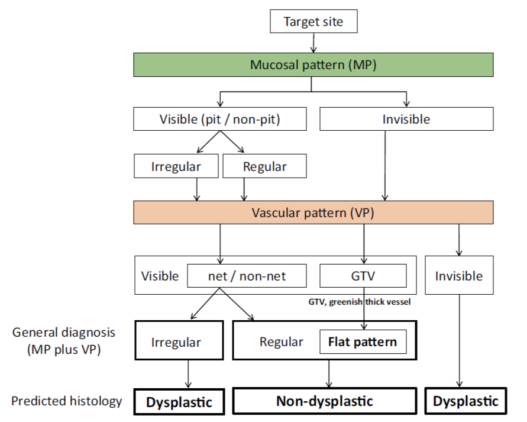
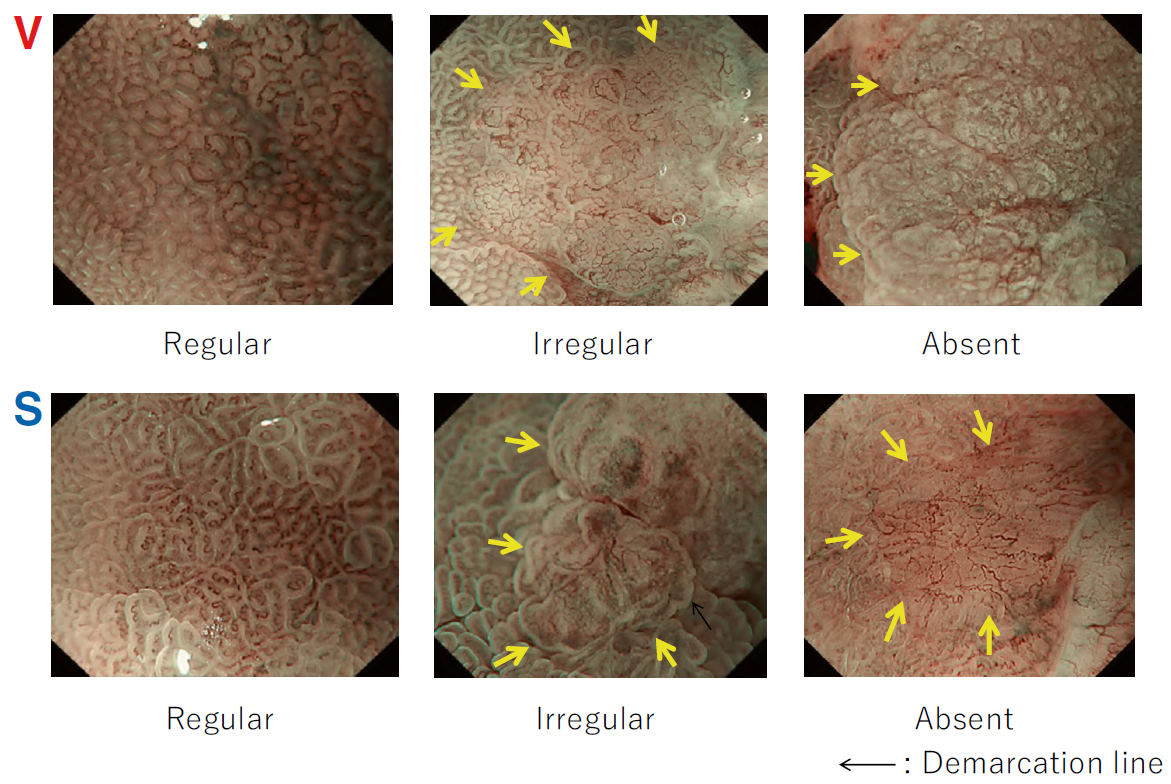
According to the morphology of the anatomical components, the MV and MS patterns were classified as regular, irregular, or absent (. Fig. 2). In principle, the MV and MS patterns must be determined separately.
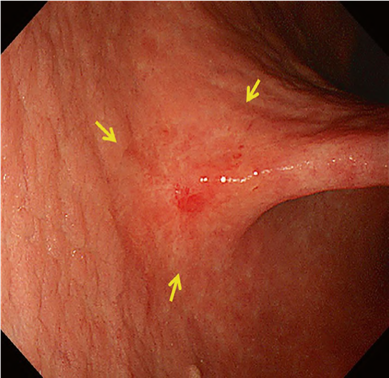
DL is defined as the border between the lesion and non-lesion areas, discernible through an abrupt change in MV and/or MS patterns (. Fig. 2).
The criteria for high-grade dysplasia (HGD)/early cancer (EC) are as follows:
- Presence of an irregular MV pattern with a demarcation line.
- Presence of an irregular MS pattern with a demarcation line.
A target lesion is diagnosed as HGD/EC if it fulfills both or either of the criteria. If it does not meet either of the criteria, it is diagnosed as noncancerous.
The diagnostic performance of M-NBI, based on the VS classification system, demonstrated excellent results with high-confidence prediction; the accuracy, sensitivity, and specificity were 98% (95% confidence interval (CI) 96.9–99.6), 85.7% (95%CI: 59.8–100), and 99.4% (95%CI: 98.2–100%), respectively [5]. Common clinical applications of M-NBI according to the VS classification system are the differential diagnosis between EGC and focal gastritis during screening endoscopy [6] and determination of the horizontal extent of EGC for successful endoscopic resection [7].
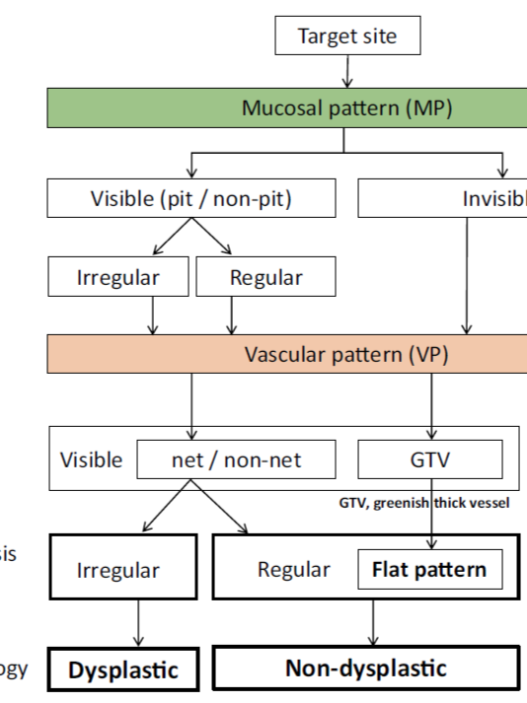
Magnifying Endoscopy Simple Diagnostic Algorithm for Gastric Cancer (MESDA-G)
Background
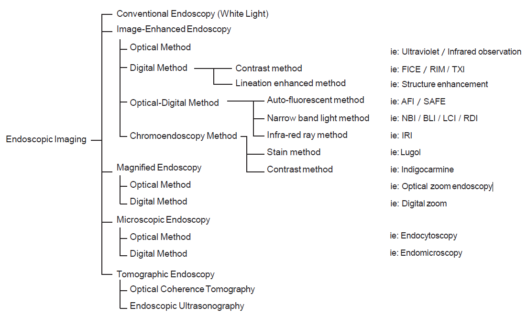
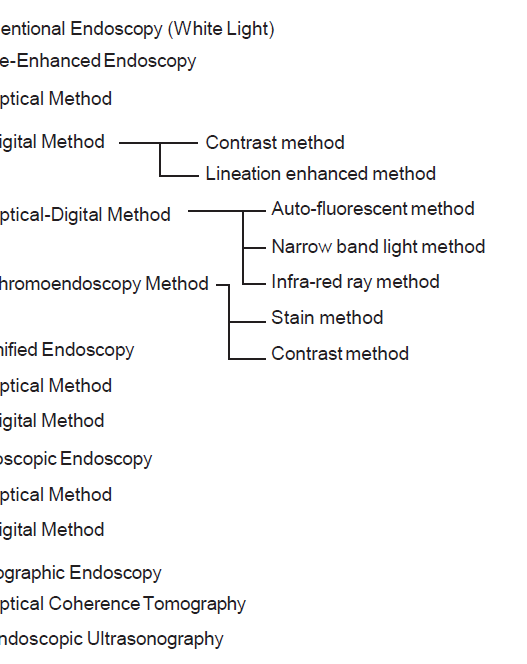
Since magnifying endoscopy (ME) has become common practice, numerous classifications and diagnostic systems have been proposed. To propose a unified algorithm for general use in clinical settings, the Japanese Gastroenterological Association established a working group and proposed that the Japan Gastroenterological Endoscopy Society, the Japanese Gastric Cancer Association, and the World Endoscopy Organization jointly devise a unified international algorithm for ME diagnosis of EGC based on an evidence-based approach.
Methods and Algorithm
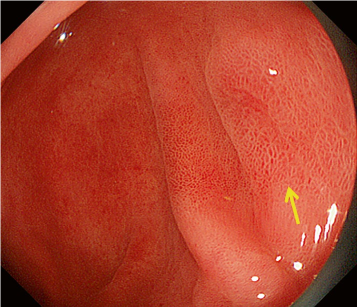
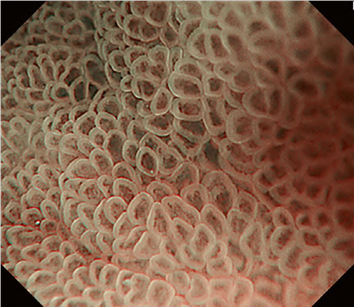
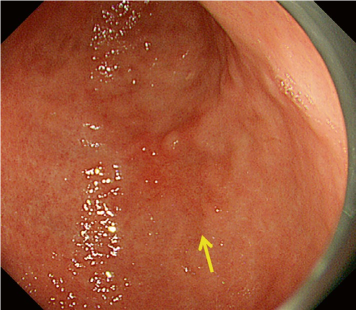
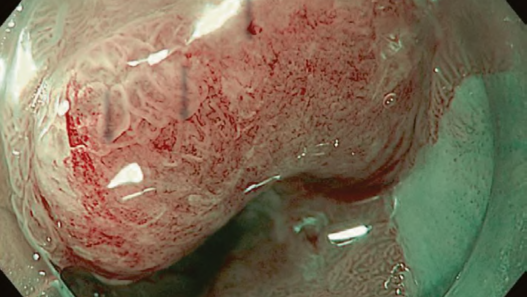
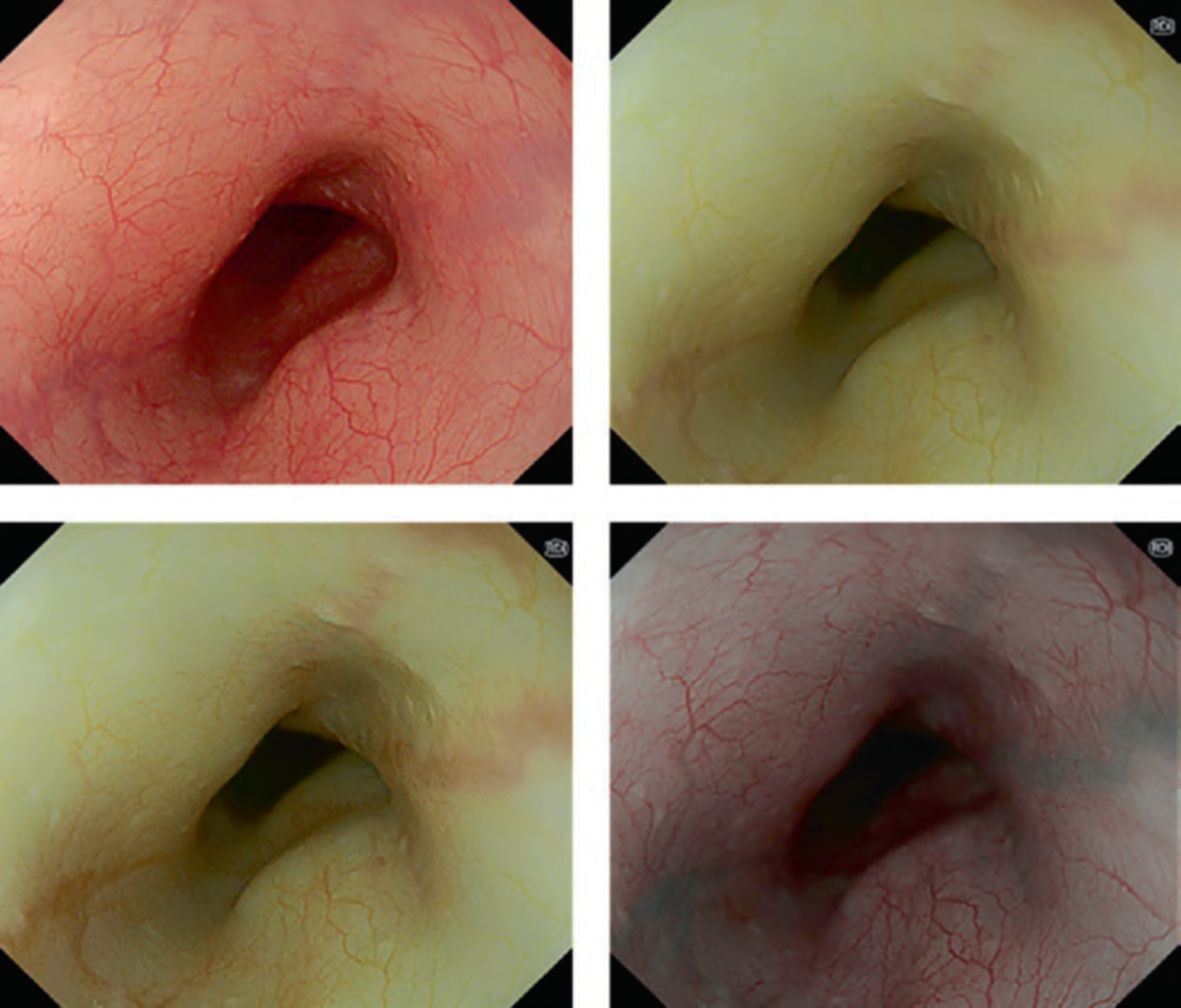
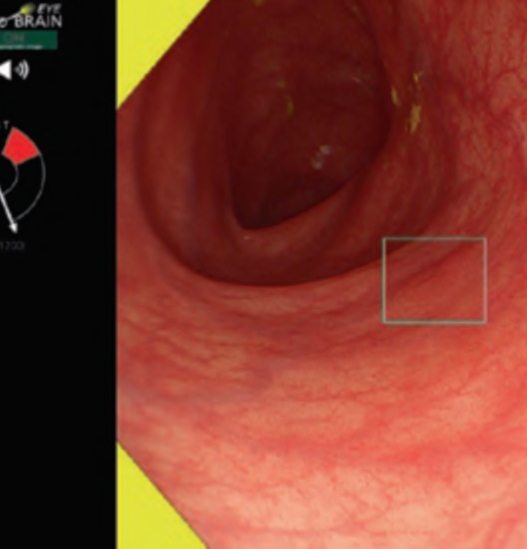
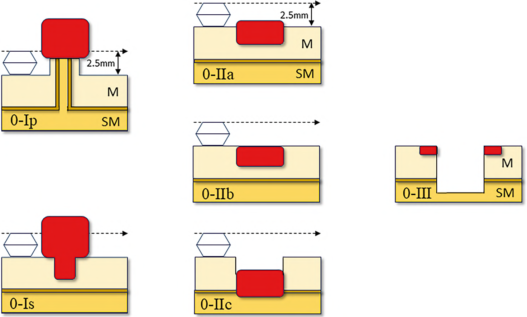
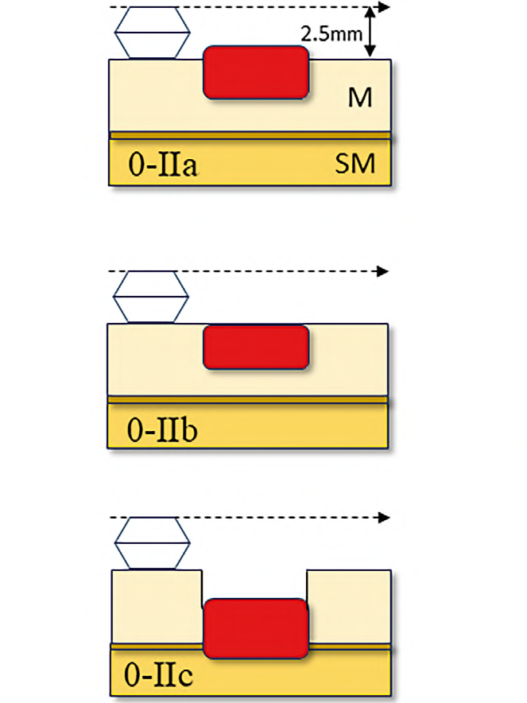
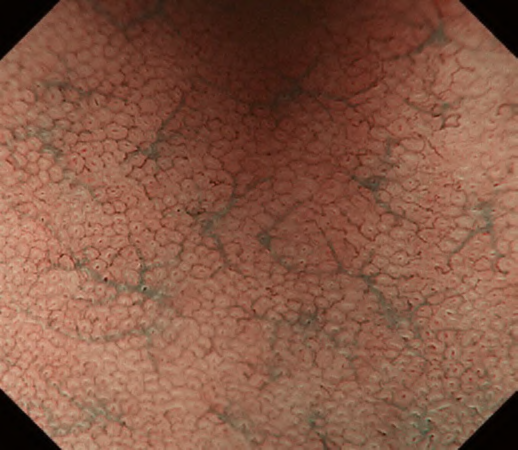
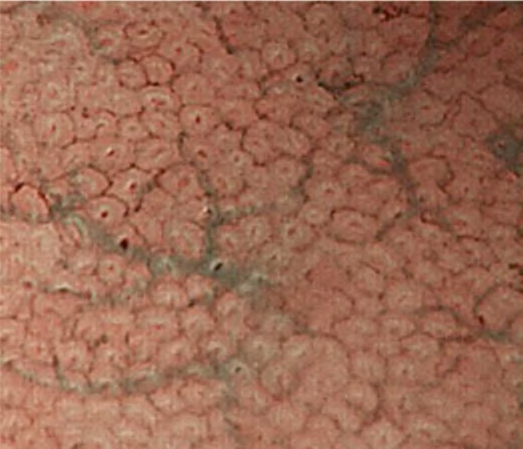
The working group members carried out a systematic review of the English literature to determine widely accepted diagnostic systems. Consequently, the best-accepted diagnostic system was proven to be the VS classification system. Based on this system, MESDA-G was constructed using an evidence-based approach (. Figs. 3, 4, 5, and 6) [2]. First, lesions suspicious for EGC should be detected by careful inspection using conventional white-light endoscopy. Subsequently, magnified observations should be performed. Owing to the high sensitivity of the demarcation line [8], if it is absent, the suspicious lesion is diagnosed as noncancerous (. Fig. 4a, b). However, if the demarcation line is present, further assessment is required to determine the presence of an irregular MV or MS pattern. If an irregular MV and/or MS pattern is detected, the suspicious lesion is diagnosed as cancerous (. Fig. 6a, b) [1, 5, 6, 8]. If both the irregular MV and MS patterns are absent, the tumor is diagnosed as noncancerous (. Fig. 5a, b) [1, 5, 6, 8].